Improving Trial Design and Reducing Costs through Biomarker Selection
Improving Trial Design
A crucial aspect of optimizing clinical trials lies in meticulously designing the study to maximize efficiency and minimize unnecessary expenditure. This involves carefully considering the patient population, the specific research question, and the available resources. Well-defined inclusion and exclusion criteria, alongside a robust statistical power analysis, are essential for ensuring the trial's ability to detect a meaningful treatment effect if one exists. Properly defined endpoints, aligned with the study objectives, are equally critical to avoid ambiguity and misinterpretations. Careful consideration of the trial's logistical aspects, such as recruitment strategies and data management protocols, also play a significant role in streamlining the process and reducing potential delays and costs.
A key element of effective trial design is the selection of appropriate study participants. This selection process should be carefully constructed to ensure the study population is representative of the patient population for whom the treatment is intended. This involves establishing clear and concise criteria for inclusion and exclusion, minimizing the risk of enrolling patients who are unlikely to benefit from the treatment or who may pose undue risk. This careful selection, supported by robust data collection methods, will help ensure the trial results are both meaningful and applicable to the target patient population, ultimately leading to a more efficient use of resources.
Reducing Costs through Biomarker Selection
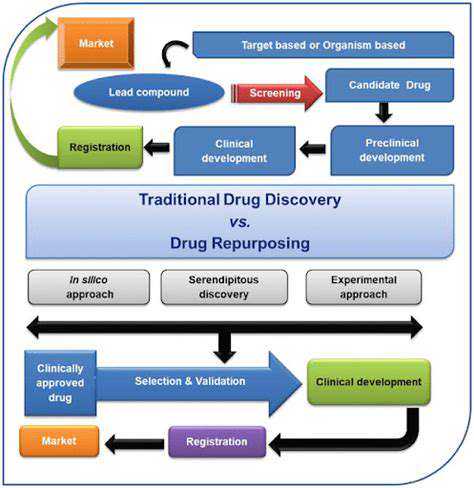
The strategic selection of biomarkers can significantly impact clinical trial costs by streamlining the process and minimizing unnecessary testing and follow-up. By identifying and prioritizing biomarkers that are strongly associated with the desired outcome, researchers can refine the study population, ensuring that only patients with a high likelihood of responding to the treatment are enrolled. This targeted approach can reduce the number of participants required to achieve statistical significance, thereby lowering the overall costs associated with recruitment, data collection, and analysis.
Biomarker selection also offers the potential to reduce the duration of the trial. When biomarkers accurately predict treatment response, researchers can potentially identify responders earlier in the trial, allowing for earlier termination of the study for non-responders. This accelerates the time to obtain valuable results, minimizing the overall time and resources invested in the trial. This efficient use of resources is critical to minimizing the financial burden of the study and accelerating the development of innovative treatments.
The Role of Biomarkers in Optimizing Trial Efficiency
Biomarkers play a pivotal role in optimizing clinical trial efficiency by providing a precise and objective means of identifying individuals who are most likely to benefit from a given treatment. The use of biomarkers allows researchers to stratify patients into cohorts based on their individual biological characteristics, enabling the development of targeted treatment strategies that are more likely to yield positive results. This approach, in turn, can reduce the number of participants required in a trial to demonstrate efficacy, thereby significantly lowering the overall cost and duration of the study.
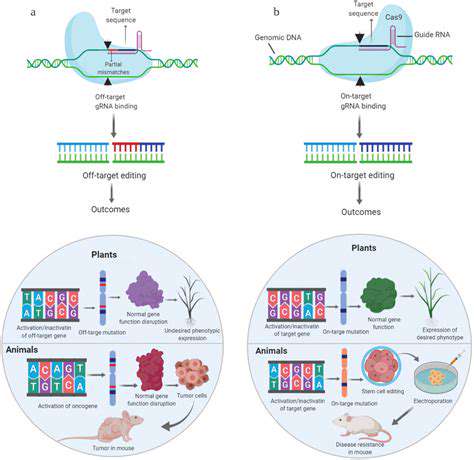
Furthermore, biomarkers can facilitate the identification of individuals who are at risk of adverse events. This proactive approach allows researchers to monitor these individuals closely and implement preventative measures, thereby reducing the risk of complications and the need for costly interventions. Early identification of potential safety concerns can lead to earlier trial termination for non-responders or those with adverse reactions, accelerating the process and reducing the overall cost of the study.
Biomarker-driven trial design can result in a more targeted approach to treatment development, leading to more effective therapies and a faster path to clinical application. This targeted approach can improve patient outcomes and accelerate the development and approval of innovative treatments, leading to a more efficient and cost-effective approach to drug development.
By incorporating biomarkers into the trial design, researchers can enhance the accuracy and reliability of the results, thereby minimizing the need for extensive follow-up studies. This enhanced precision can improve the efficiency of the overall research process by reducing the time and resources needed to obtain meaningful results.
The ability to use biomarkers to predict response to treatment is crucial in minimizing the costs associated with recruiting and enrolling patients who are unlikely to benefit from the intervention. This allows for a more targeted approach to patient selection, reducing the overall cost of the trial.
Ultimately, the thoughtful selection and integration of biomarkers into clinical trial design contributes to a more efficient, cost-effective, and ultimately, impactful research process.
The Future of Biomarkers in Personalized Medicine
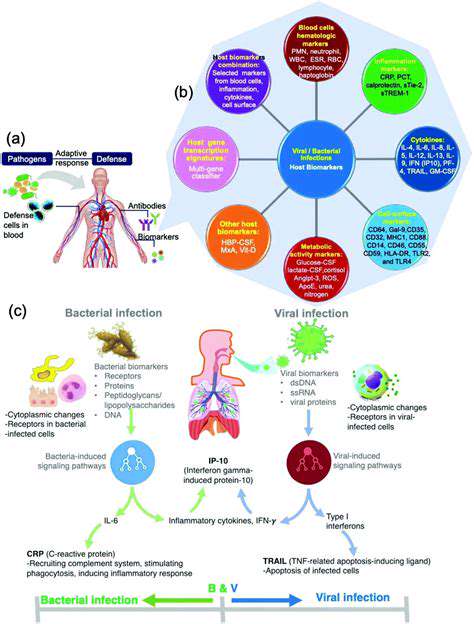
The Expanding Role of Biomarkers in Precision Diagnosis
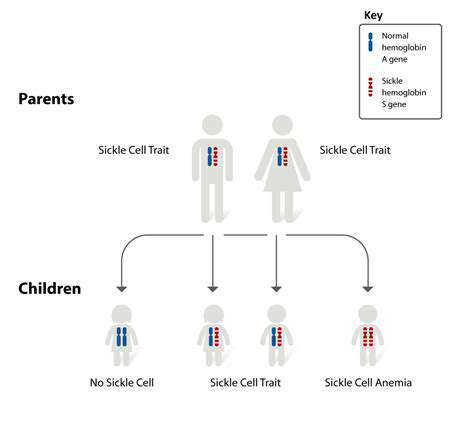
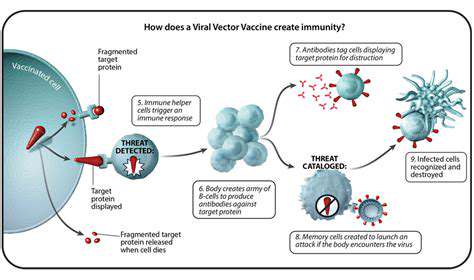
Biomarkers are rapidly becoming integral to personalized medicine, enabling clinicians to diagnose diseases with greater accuracy and precision. Their ability to detect subtle changes in biological processes allows for earlier intervention and tailored treatment plans. This shift towards precision diagnosis, leveraging biomarker data, is revolutionizing healthcare by moving away from a one-size-fits-all approach and moving towards a more individualized approach to patient care.
By identifying specific molecular signatures, biomarkers facilitate the identification of individuals at risk for developing certain diseases. This proactive approach allows for preventive measures to be implemented, potentially mitigating the severity of disease progression and improving overall health outcomes. Early detection enables timely intervention, potentially preventing the development of debilitating conditions.
Personalized Treatment Strategies Based on Biomarker Profiles
Beyond diagnostic applications, biomarkers are instrumental in guiding personalized treatment strategies. Analyzing a patient's unique biomarker profile allows physicians to select the most effective treatment regimen, minimizing adverse reactions and maximizing therapeutic efficacy. This approach is particularly crucial in oncology, where different cancers exhibit varying responses to specific therapies.
Precise understanding of a patient's genetic makeup, combined with biomarker data, empowers physicians to select the most appropriate medication, dosage, and schedule, tailoring treatment to individual needs and reducing the risk of ineffective or harmful treatments. This personalized approach to treatment selection is a major advancement in healthcare.
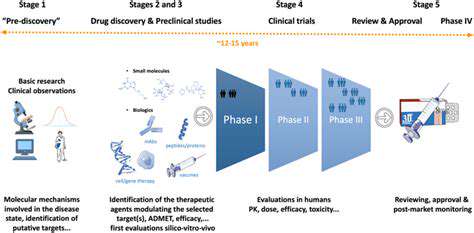
Improving Drug Development and Efficacy Through Biomarker Selection
The selection of appropriate biomarkers in drug development is crucial for identifying potential candidates for clinical trials. By focusing on patients with specific biomarker profiles, pharmaceutical companies can streamline the drug development process, reducing costs and accelerating the identification of effective therapies. This targeted approach ensures clinical trials are more likely to yield positive results, accelerating the path to new and improved treatments.
Biomarker profiling plays a critical role in ensuring that clinical trials are focused on patients who are most likely to respond to the drug being tested. This efficiency translates into significant cost savings and faster time to market for new therapies. Ultimately, selecting the right patients for clinical trials, based on biomarker profiles, is key to accelerating the development of effective treatments.
The Impact of Biomarkers on Minimizing Adverse Reactions
Biomarkers can significantly contribute to minimizing adverse drug reactions (ADRs). By identifying patients predisposed to specific side effects, physicians can adjust treatment strategies to mitigate potential harm. This proactive approach to patient care improves treatment outcomes and enhances patient safety.
The ability to predict potential adverse drug reactions based on a patient's biomarker profile allows for preventive measures to be put in place. This approach can reduce the frequency and severity of adverse events, leading to a more comfortable and effective treatment experience for patients. Early identification of potential issues ensures that appropriate interventions can be employed.
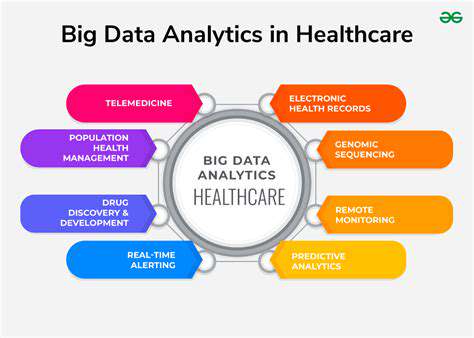
Integrating Biomarker Data into Electronic Health Records (EHRs)
The seamless integration of biomarker data into electronic health records (EHRs) is essential for creating comprehensive patient profiles. This integration facilitates efficient data sharing among healthcare providers, enabling better communication and improved coordination of care. The centralized storage of biomarker information within EHRs enhances accessibility and facilitates the effective use of this data in clinical decision-making.
Ethical Considerations and Data Security in Biomarker Research
The increasing use of biomarkers in personalized medicine necessitates careful consideration of ethical implications, including issues of data privacy and security. Robust measures to protect patient confidentiality and ensure responsible data handling are paramount. Ensuring the ethical collection, storage, and usage of biomarker data is crucial to maintain public trust and confidence in this evolving field.
The development of stringent data security protocols is essential to protect sensitive patient information associated with biomarker analysis. This protection safeguards patient privacy and ensures that the data is used responsibly and ethically. Careful attention to the ethical and regulatory aspects of biomarker research is paramount to the long-term success and acceptance of this technology.
The Future of Biomarker Research in Personalized Oncology
The application of biomarkers is particularly promising in oncology, where personalized treatment strategies are crucial for improving cancer patient outcomes. Understanding the specific genetic and molecular characteristics of each cancer type, using biomarkers, allows for more targeted and effective therapies. This personalized approach holds the key to improving survival rates and treatment responses in cancer patients.