Inherited Retinal Degenerations: A Growing Challenge
Inherited retinal diseases (IRDs) represent a collection of genetically diverse conditions that impair the retina, the delicate tissue at the eye's rear responsible for capturing light. These disorders can cause gradual vision deterioration, from minor disturbances to total blindness. The genetic anomalies behind these diseases are highly varied and intricate, complicating both diagnosis and therapeutic approaches. Pinpointing the exact genetic mutations is essential for crafting targeted treatments, particularly those involving gene editing.
Treating IRDs faces a major obstacle due to the retina's complex cellular architecture. The precise interplay between retinal cells and their connections to the optic nerve demands interventions that are both accurate and potent. Current treatment avenues for IRDs remain scarce, underscoring the pressing need for groundbreaking solutions like gene therapy.
Gene Therapy Strategies for Vision Restoration
Gene therapy offers a beacon of hope for IRD treatment. This method focuses on replacing or repairing defective genes to reinstate normal retinal activity. Scientists are investigating multiple gene therapy techniques, such as viral vectors designed to transport healthy genes to specific retinal cells. These vectors are meticulously engineered to ensure the right genes reach their intended destinations.
By introducing functional gene copies, gene therapy seeks to revive the production of vital proteins needed for retinal health. This strategy could potentially stop or even reverse vision loss in IRD patients.
CRISPR/Cas9 Technology: A Revolutionary Tool
CRISPR/Cas9 has emerged as a game-changing gene-editing tool for IRDs. It enables scientists to make exact modifications to specific DNA segments within the genome. Such precision is indispensable for correcting genetic errors in IRDs without disrupting unrelated genetic material.
Challenges and Future Directions in Gene Therapy
Despite its promise, gene therapy faces hurdles. Ensuring therapeutic genes reach the correct retinal cells and maintain long-term expression is critical for sustained benefits. Ongoing research aims to refine these aspects of gene therapy protocols.
Safety remains a top priority. Potential off-target effects and immune reactions must be meticulously studied and mitigated. Clinical trials are currently evaluating the safety and effectiveness of gene therapy for IRDs, laying the groundwork for future treatments.
Ethical Considerations and Public Health Implications
The rise of gene-editing technologies like CRISPR brings ethical questions to the forefront. Discussions must address societal impacts and ensure fair access to these treatments. Public health concerns, including the implications of germline editing, demand thorough debate and regulatory oversight.
Establishing ethical guidelines is essential for the responsible advancement of gene therapy for IRDs. Transparency and public involvement are key to building trust and addressing concerns about this transformative technology. Engaging patients, researchers, policymakers, and the public ensures gene therapy is used ethically and effectively to enhance the lives of those affected by IRDs.
Beyond Retinal Diseases: Addressing Other Vision Challenges

Beyond the Retina: A Broader Perspective
While retinal diseases are significant, they represent only part of the broader eye health spectrum. A holistic approach to eye care must consider the entire ocular system, including the optic nerve, cornea, lens, and supporting structures. Each component plays a critical role in vision.
Environmental factors and systemic health conditions also profoundly influence eye health. Recognizing these connections is vital for developing proactive strategies to preserve ocular well-being and prevent potential issues.
The Importance of Early Detection
Early detection and intervention are crucial for managing eye conditions effectively, regardless of their location. Timely diagnosis and treatment can often halt or slow disease progression, leading to better outcomes and minimizing long-term damage.
Many eye conditions, if caught early, can be managed or even reversed, significantly improving patients' quality of life.
Addressing Systemic Health Factors
Overall health directly impacts eye health. Conditions like diabetes, hypertension, and autoimmune disorders elevate the risk of eye complications. Proactively managing these systemic issues is essential for preventing ocular damage.
Regular visits to both ophthalmologists and primary care physicians are key to identifying and controlling these systemic factors, ensuring comprehensive patient care.
Innovative Diagnostic Techniques
Advances in diagnostic technology are revolutionizing eye disease detection. Cutting-edge tools enable earlier, more accurate diagnoses, paving the way for improved treatment plans and better patient outcomes.
State-of-the-art imaging and genetic testing offer unparalleled insights into eye diseases, accelerating the development of more effective therapies.
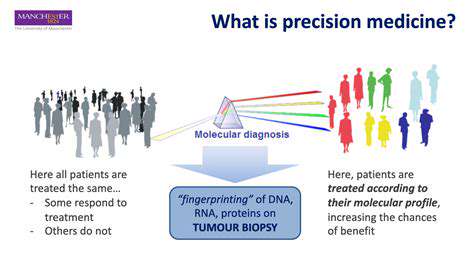
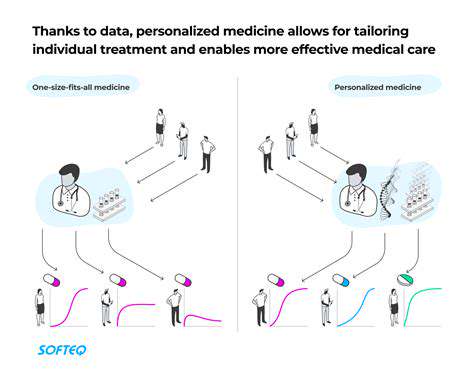
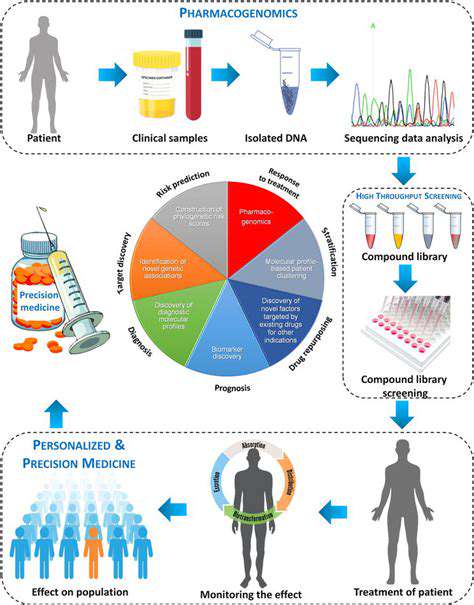
Personalized Treatment Approaches
Tailoring treatments to individual patients is becoming increasingly important in eye care. Customized plans that account for medical history, lifestyle, and genetic factors are essential for optimal results.
This patient-centered approach considers both the disease and overall health, leading to more effective treatments and enhanced long-term outcomes.
The Future of Gene Editing in Ophthalmology: Hope and Progress
Harnessing CRISPR-Cas9 for Retinal Disease
CRISPR-Cas9 stands at the forefront of ophthalmic innovation, offering potential cures for various retinal diseases. This technology allows precise DNA modifications, potentially correcting mutations behind conditions like retinitis pigmentosa and macular dystrophy. Preclinical studies show promising results, with CRISPR-Cas9 successfully restoring retinal cell function and paving the way for personalized medicine.
Developing safe, efficient delivery systems for CRISPR-Cas9 components is critical for clinical translation. Researchers are testing viral vectors and lipid nanoparticles to ensure the technology's safety and efficacy, addressing key challenges for its widespread use.
Beyond CRISPR: Exploring Novel Gene Editing Strategies
While CRISPR-Cas9 dominates the field, alternatives like base editing and prime editing are gaining traction. Base editing allows single-base DNA changes without double-strand breaks, potentially reducing unintended effects. Prime editing enables more complex modifications, broadening the scope of correctable genetic defects.
These innovations may overcome CRISPR-Cas9 limitations, such as off-target effects and delivery challenges in the eye's complex structure. Further research will determine their viability for ophthalmic applications.
Clinical Trials and Regulatory Hurdles
Transitioning from lab to clinic is a critical step for gene editing therapies. Ongoing clinical trials are assessing CRISPR-Cas9 and other approaches for retinal diseases, evaluating their safety and effectiveness. The rigorous regulatory process is vital for patient safety and treatment longevity.
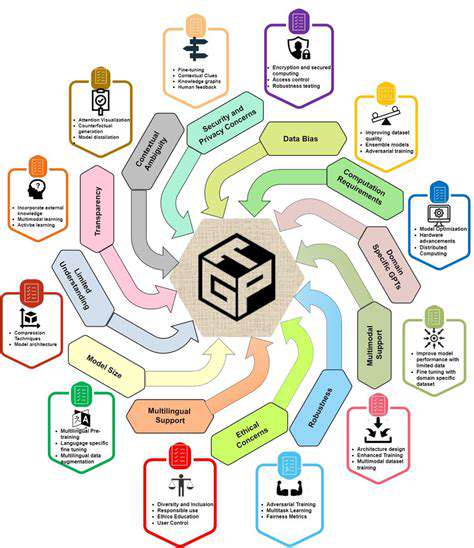
Navigating ethical and regulatory landscapes remains challenging. Debates over long-term effects and equitable access must be resolved to ensure responsible use of these technologies in ophthalmology.
Ethical Considerations and Future Directions
The rapid evolution of gene editing raises ethical questions about unintended consequences and fair access. Collaboration among scientists, ethicists, and policymakers is essential to establish guidelines for responsible development and use. Public engagement and transparency will foster trust in these powerful tools.
Future directions include personalized treatments, expanding gene editing to other eye diseases, and integrating it with other therapies. Continued research and ethical oversight will unlock gene editing's full potential in ophthalmology.