Empowering Natural Immunity Against Cancer
Modern immunotherapy techniques have fundamentally changed oncology by leveraging the patient's own immune defenses. This paradigm shift moves beyond conventional treatments by training immune cells to specifically recognize and eliminate malignant cells, often with remarkable precision. The beauty of this approach lies in its ability to potentially create durable responses through immune memory.
When comparing treatment modalities, chemotherapy often acts like a blunt instrument, while immunotherapy functions more like a precision-guided system. The targeted nature of immune-based treatments frequently results in better tolerability profiles, allowing patients to maintain daily activities during therapy.
Understanding Immunotherapeutic Mechanisms
The science behind these treatments involves sophisticated biological interactions. Researchers have identified multiple pathways to enhance immune surveillance against tumors, with each method offering unique advantages.
Checkpoint inhibitors represent a breakthrough by essentially removing cancer cells' ability to hide from immune detection. These drugs target molecular off switches that tumors exploit to avoid destruction, effectively unleashing T-cells to attack malignancies.
Diverse Immunotherapy Approaches
The therapeutic arsenal continues to expand with innovative techniques. CAR-T cell therapy exemplifies this progress, where a patient's lymphocytes are genetically reprogrammed to better identify cancer-specific markers before being reintroduced to circulate throughout the body.
Navigating Treatment Complexities
Despite remarkable successes, immunotherapy presents unique management challenges. Response patterns show significant variation between patients, with some experiencing dramatic tumor regression while others show limited benefit. This variability underscores the need for predictive biomarkers.
Immune-related adverse events require careful monitoring as they can affect multiple organ systems. These effects occur when activated immune cells mistakenly attack healthy tissues, necessitating prompt intervention to maintain treatment safety.
Innovations on the Horizon
Current investigations focus on improving response predictability and duration. Emerging technologies aim to enhance tumor antigen recognition while minimizing off-target effects, potentially through combination approaches or novel delivery systems.
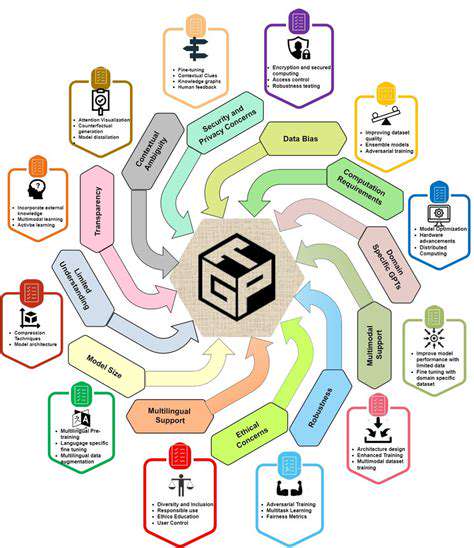
The next generation of immunotherapies may incorporate artificial intelligence to personalize treatment regimens based on individual tumor profiles, representing a significant leap toward precision medicine in oncology.
Clinical Evidence and Practical Applications
Notable successes have been documented in treating aggressive cancers that previously had limited options. Some patients with advanced melanoma or non-small cell lung cancer have achieved long-term disease control previously thought impossible.
Treatment selection requires comprehensive evaluation of tumor characteristics, patient physiology, and available immunotherapeutic options. Multidisciplinary teams often collaborate to determine optimal sequencing with other modalities like radiation or surgery.
Modern machine learning applications demonstrate parallel evolution in adaptive systems. Just as online learning algorithms continuously adjust to new data inputs, immunotherapy regimens are increasingly designed to adapt based on patient response monitoring. This dynamic approach represents the future of personalized medicine across disciplines.
Combination Therapies: Strategic Synergy in Medical Treatment
The Science of Therapeutic Synergy
Contemporary combination approaches strategically integrate multiple agents to attack diseases through complementary mechanisms. This multidimensional strategy often achieves superior outcomes by addressing various pathological pathways simultaneously while potentially reducing individual drug toxicities.
The rationale behind these regimens involves careful selection of agents that work through distinct but complementary mechanisms. For instance, one component might inhibit tumor blood vessel formation while another directly targets cancer cell replication. Such strategic pairings can produce effects greater than simple additive benefits.
Designing Optimal Treatment Cocktails
Developing effective combinations requires meticulous pharmacological planning. Scientists must consider how drugs interact at molecular levels, including potential effects on each other's metabolism and distribution patterns within the body.
An equally critical consideration involves preventing or delaying resistance development. Multi-target approaches inherently create higher evolutionary barriers for pathogens or cancer cells to overcome, making resistance less probable compared to single-agent therapies.
Current Applications and Emerging Possibilities
Clinical practice already incorporates many successful combination regimens. Oncology frequently pairs cytotoxic drugs with molecular targeted agents, while infectious disease management routinely uses antimicrobial combinations to prevent resistance emergence.
Future directions include sophisticated computational modeling to predict optimal drug pairs and advanced screening platforms to evaluate thousands of potential combinations. These technological advances promise to accelerate the discovery of novel therapeutic synergies across medical specialties.