Personalized medicine is transforming healthcare by moving away from a one-size-fits-all approach to treating diseases. This revolutionary approach considers individual factors like genetics, lifestyle, and environment to create tailored treatment plans. This shift promises more effective therapies and reduced side effects, ultimately leading to better health outcomes. This approach is particularly valuable in tackling complex diseases like cancer, where genetic variations play a crucial role in disease progression and response to treatment.
It's a paradigm shift from treating symptoms to understanding the underlying causes of disease within each patient. This personalized approach is not just about adjusting dosages; it's about tailoring the entire treatment strategy to the unique characteristics of the individual.
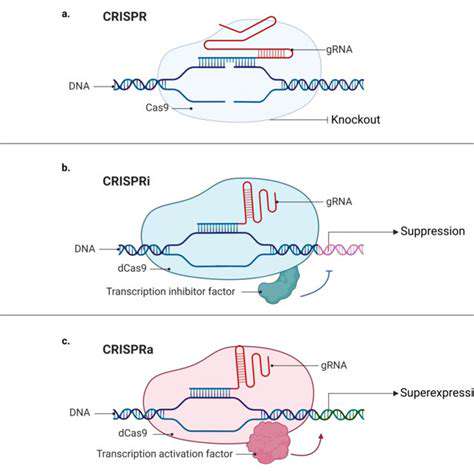
Targeted Therapies: Precision at its Finest
Targeted therapies are a core component of personalized medicine. These therapies focus on specific molecules or pathways within the body involved in disease development. By identifying these specific targets, doctors can design treatments that specifically attack the disease without harming healthy cells. This precision approach minimizes side effects and maximizes the effectiveness of treatment.
This targeted approach is particularly effective in cancer treatment, where specific genetic mutations drive the growth of tumors. By targeting these mutations, doctors can effectively eliminate cancer cells while minimizing damage to healthy tissues.
Genetic Factors and Disease Susceptibility
Genetic predispositions significantly influence an individual's risk of developing certain diseases. Understanding an individual's genetic makeup allows healthcare providers to identify potential vulnerabilities and tailor preventative measures. This proactive approach allows for early intervention and potentially prevents the onset of the disease.
Lifestyle Factors and Health Outcomes
Lifestyle choices, such as diet, exercise, and stress management, play a crucial role in overall health and disease risk. Personalized medicine takes these factors into consideration, creating individualized plans that promote healthy habits and improve overall well-being. This focus on lifestyle factors empowers patients to take an active role in their health management.
By understanding how lifestyle choices interact with genetic predispositions, healthcare professionals can provide more effective and comprehensive care, leading to improved health outcomes.
Pharmacogenomics: Tailoring Medications to Individuals
Pharmacogenomics is a crucial aspect of personalized medicine. It studies how an individual's genetic makeup affects their response to medications. By understanding these genetic variations, doctors can predict how a patient will respond to a particular drug, thus choosing the most effective medication and dosage. This approach significantly reduces the risk of adverse drug reactions.
Diagnostics and Early Detection
Advanced diagnostic tools, such as genetic testing and imaging technologies, are essential components of personalized medicine. These tools allow for early detection of diseases, enabling timely intervention and improving treatment outcomes. Early detection can significantly increase the chances of successful treatment. This proactive approach also allows for the implementation of preventative strategies.
Personalized medicine is not just about treatment; it's about understanding the patient's unique needs and tailoring the approach accordingly. This proactive approach to healthcare focuses on prevention, early intervention, and precision treatment, leading to better health outcomes.
The Future of Personalized Medicine
The field of personalized medicine is constantly evolving, driven by advancements in technology and research. Future innovations promise even more precise diagnoses and treatments, leading to a future where healthcare is truly customized to the individual. This innovative approach is poised to revolutionize the healthcare industry, offering more effective and personalized care to patients worldwide.
The ongoing research in this field will likely lead to more effective treatments and prevention strategies, ultimately improving the quality of life for everyone.
Intrinsic motivation, the drive to engage in an activity for its inherent satisfaction, plays a crucial role in fostering long-term engagement. It's a powerful force that stems from within, driven by a genuine interest in the task itself, a sense of accomplishment, or a desire for personal growth. Understanding the factors that ignite intrinsic motivation is essential for creating an environment where individuals are actively invested in their work or learning. This type of engagement goes beyond external rewards and focuses on the inherent satisfaction derived from the activity.
Overcoming Challenges and Future Directions
Addressing Financial Constraints in Oncology Drug Discovery
One of the significant hurdles in oncology drug discovery is the substantial financial investment required. Developing novel therapies often entails years of research, extensive clinical trials, and regulatory approvals – all of which demand substantial financial resources. Securing funding from various sources, including government grants, private investment, and philanthropic contributions, is crucial for advancing promising drug candidates. Finding innovative ways to streamline research processes and reduce development timelines can also contribute to lowering the overall cost of drug discovery.
Furthermore, the high failure rate of clinical trials further exacerbates the financial burden. Developing robust preclinical models and incorporating more sophisticated analytical tools in the early stages of research can help mitigate this risk. Partnerships between pharmaceutical companies, academic institutions, and biotech startups can leverage resources and expertise, potentially leading to more efficient and effective drug discovery strategies.
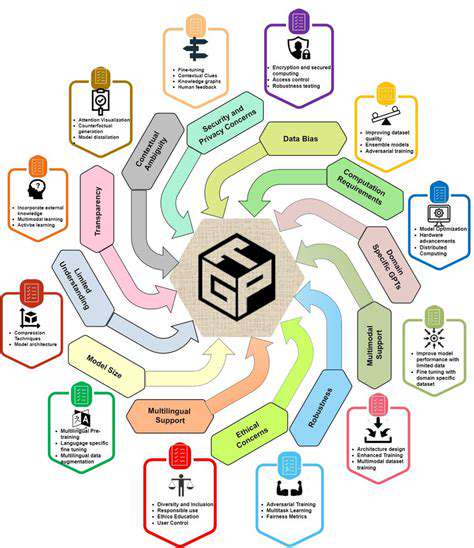
Harnessing the Power of Artificial Intelligence in Drug Design
Artificial intelligence (AI) is rapidly transforming various fields, including drug discovery. AI algorithms can analyze vast datasets of biological information, identify potential drug targets, and predict the efficacy and safety profiles of novel compounds. This can significantly accelerate the drug discovery process, reducing the time and resources needed to identify promising candidates.
Machine learning techniques can also help optimize existing drug designs, leading to improved efficacy and reduced side effects. By integrating AI into the drug discovery pipeline, researchers can explore a broader range of possibilities and potentially discover innovative therapies more effectively.
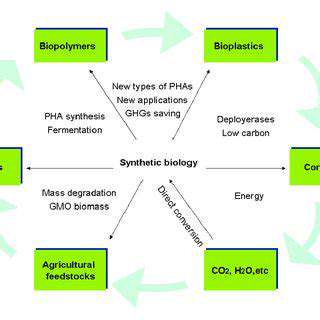
Improving Preclinical Modeling for Oncology Therapies
Accurate and reliable preclinical models are essential for evaluating the efficacy and safety of potential oncology therapies. Current models, while valuable, often fail to fully replicate the complexity of human cancers. Developing more sophisticated models that incorporate genetic and environmental factors, as well as the tumor microenvironment, can provide a more accurate reflection of the disease process.
Advanced technologies, such as 3D organoid cultures and personalized patient-derived xenograft models, can help researchers better understand the response of cancer cells to potential therapies. This enhanced understanding can lead to the identification of more effective and less toxic treatment strategies.
Overcoming Resistance Mechanisms in Cancer Cells
Cancer cells often develop resistance mechanisms that limit the effectiveness of existing therapies. Understanding the molecular mechanisms behind drug resistance is crucial for developing strategies to overcome these hurdles. Researchers are actively investigating various approaches, including the development of combination therapies, targeting multiple pathways simultaneously, and modulating the tumor microenvironment.
Enhancing Patient Recruitment and Retention in Clinical Trials
Efficiently recruiting and retaining patients in clinical trials is vital for evaluating the efficacy and safety of new therapies. Improving patient engagement through clear communication, accessible trial information, and supportive care systems can help improve recruitment rates. Furthermore, addressing the diverse needs of diverse populations is crucial to ensure trial participation is representative of the patient population.
Utilizing innovative recruitment strategies, such as technology-based platforms and community partnerships, can help broaden the reach of clinical trials and increase patient participation. Addressing potential barriers to participation, such as cost, logistical challenges, and cultural factors, is crucial for successful trial recruitment and retention.
Promoting Interdisciplinary Collaboration in Drug Discovery
Oncology drug discovery is a complex process that requires expertise from various disciplines. Promoting interdisciplinary collaboration between researchers, clinicians, and other stakeholders can foster a more holistic approach to drug development. Bringing together specialists in oncology, pharmacology, chemistry, and bioinformatics can lead to innovative solutions and breakthroughs.
Creating collaborative research environments, sharing data and resources, and fostering a culture of knowledge exchange can further enhance the effectiveness and efficiency of drug discovery initiatives. Open access to data and research tools can accelerate the pace of discovery and help researchers worldwide contribute to the fight against cancer.