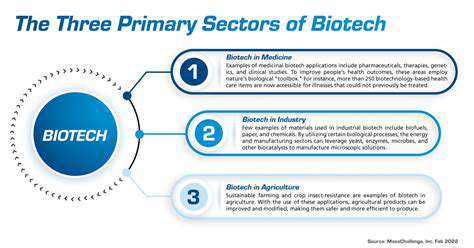
Biomarker Identification and Validation
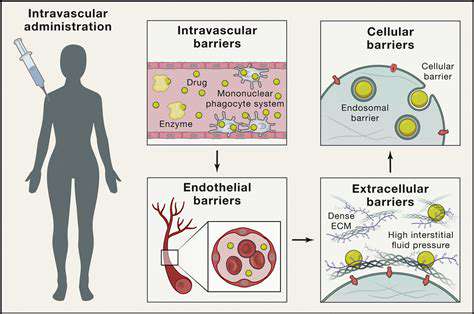
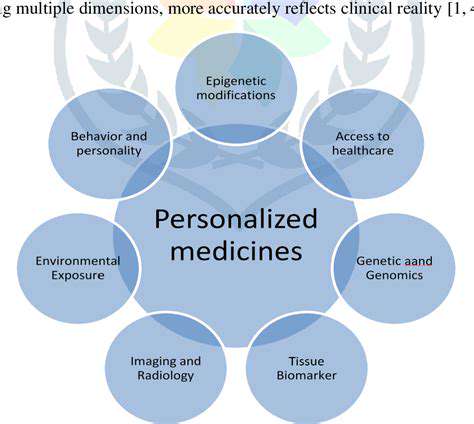
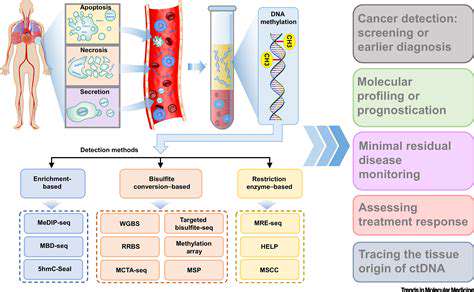
Identifying reliable biomarkers is crucial for accurate disease diagnosis and prognosis. Biomarkers, measurable indicators of biological processes, can provide valuable insights into the presence, progression, or response to treatment of various diseases. This process often involves extensive research and rigorous validation to ensure the biomarker's specificity and sensitivity in detecting the target condition. Validation studies typically compare the biomarker's performance against established diagnostic methods, and involve large sample sizes to account for variability.
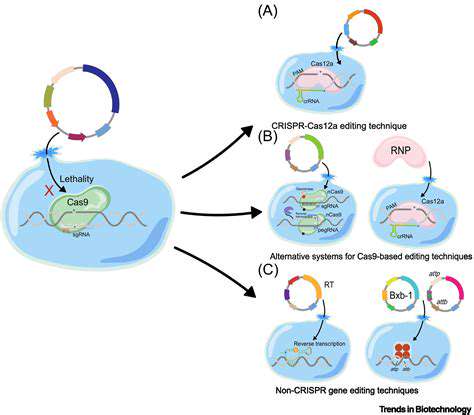
The identification of novel biomarkers often relies on sophisticated analytical techniques, such as proteomics, genomics, and metabolomics. These techniques allow researchers to explore complex biological systems and identify potential biomarkers that might not be readily apparent using traditional methods. Furthermore, understanding the underlying mechanisms that link the biomarker to the disease is essential for developing effective diagnostic and therapeutic strategies.
Diagnostic Applications of Biomarkers
Biomarkers are transforming the landscape of diagnostics, enabling earlier and more precise disease detection. Early detection is often critical for optimizing treatment outcomes, especially in conditions like cancer. These advancements in diagnostics are leading to more personalized and targeted therapies, enhancing patient care and improving overall health outcomes. For example, certain biomarkers can predict an individual's risk of developing specific diseases, allowing for proactive interventions and preventive measures.
The development of point-of-care diagnostic tools based on biomarkers is rapidly advancing. These tools enable quick and convenient testing, making diagnosis more accessible and efficient, particularly in resource-limited settings. This accessibility is a major advantage, offering the potential for widespread implementation and early intervention.
Challenges and Future Directions
Despite significant progress, several challenges remain in the field of biomarker-based diagnostics. One key challenge involves the cost-effectiveness and scalability of biomarker assays, particularly for large-scale clinical applications. Developing cost-effective and reliable diagnostic tests is essential to widespread adoption. Furthermore, ensuring the ethical considerations and data privacy associated with biomarker-based diagnostics is crucial.
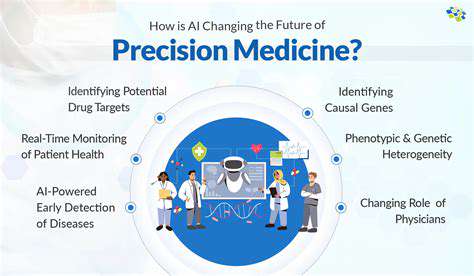
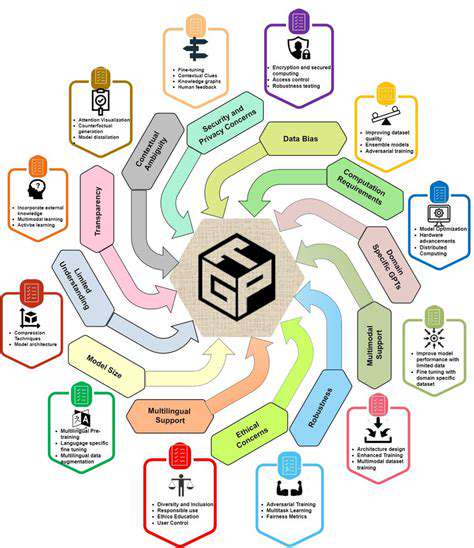
Future research will focus on developing more sophisticated and accurate biomarker panels for complex diseases. The integration of artificial intelligence and machine learning techniques will likely play a critical role in analyzing complex data sets, leading to more accurate and personalized diagnostics.
Technological Advancements in Biomarker Research
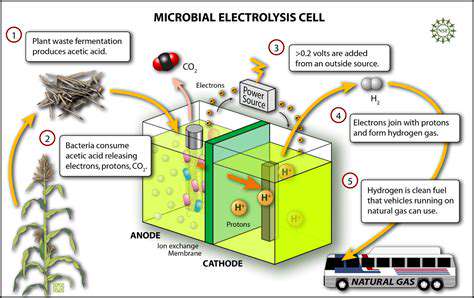
Technological advancements are driving progress in biomarker discovery and validation. Next-generation sequencing technologies are providing unprecedented insights into the genomic landscape of diseases, paving the way for the identification of novel biomarkers. This improved understanding is leading to development of new diagnostic strategies. Advances in microfluidic technology are crucial for developing miniaturized and portable diagnostic devices, making testing more accessible and affordable.
Furthermore, the use of bioinformatics tools and computational modeling is facilitating the analysis and interpretation of vast amounts of data generated from various omics technologies. This analysis is essential for identifying patterns and correlations among different biomarkers. This sophisticated approach is crucial for the development of robust and reliable diagnostic tools.
Ethical Considerations and Future Directions

Ethical Implications of AI in Healthcare
The integration of artificial intelligence (AI) into healthcare presents a plethora of ethical dilemmas that require careful consideration. AI systems, while capable of enhancing diagnostic accuracy and treatment efficacy, also raise concerns about patient privacy and data security. The potential for bias in algorithms trained on existing data could lead to disparities in care, affecting vulnerable populations disproportionately. It is crucial to establish robust ethical guidelines and regulations to mitigate these risks and ensure equitable access to AI-powered healthcare for all.
Furthermore, questions arise regarding the responsibility for errors made by AI systems. Determining liability in cases of misdiagnosis or inappropriate treatment recommendations necessitates careful legal frameworks. Transparency in AI decision-making processes is essential to allow clinicians and patients to understand the reasoning behind AI-generated recommendations, fostering trust and accountability. This transparency also aids in identifying and mitigating potential biases within the algorithms.
Ensuring Equitable Access to AI-Powered Healthcare
One significant ethical consideration is ensuring equitable access to AI-powered healthcare solutions. The cost of implementing AI technologies in healthcare settings may create disparities between affluent and underserved communities, potentially exacerbating existing health inequities. Efforts to develop and deploy AI tools in a manner that promotes affordability and accessibility across diverse populations are crucial. This necessitates innovative financing models and strategies for widespread adoption.
Another critical aspect is the need to address the digital divide and ensure equitable access to the technology and digital literacy necessary to utilize AI tools effectively. Education and training programs targeting underserved communities are essential to bridge this gap and enable broader participation in the benefits of AI-driven healthcare.
The Future of AI in Healthcare: A Multifaceted Approach
The future of AI in healthcare is promising, but its successful integration requires a multifaceted approach. This involves not only developing sophisticated AI algorithms but also addressing the ethical, social, and economic implications. Collaboration between healthcare professionals, AI developers, policymakers, and ethicists is paramount to navigating the complexities of this transformative technology. This collaborative effort should focus on establishing clear ethical guidelines, fostering public trust, and ensuring responsible development and deployment of AI tools.
Ultimately, the goal is to utilize AI to augment, rather than replace, human expertise. By developing AI tools that complement clinical judgment and improve patient outcomes, we can harness the power of this technology for the benefit of all. This partnership between humans and machines holds immense potential to revolutionize healthcare, providing more personalized, efficient, and accessible care for everyone.
The integration of AI into healthcare requires careful consideration of long-term implications. This includes anticipating potential job displacement within the healthcare sector and designing retraining programs to support affected individuals. Continuous monitoring and evaluation of AI systems are essential to ensure their effectiveness and alignment with ethical principles. Addressing the ongoing challenges of data privacy, algorithmic bias, and cost-effectiveness is crucial to realizing the full potential of AI in healthcare.
Addressing these complexities will be crucial to building a sustainable and beneficial future for AI in healthcare.