Harnessing the Power of Gene Editing
Gene editing technologies, particularly CRISPR-Cas9 systems, represent a paradigm shift in medical treatment possibilities. These molecular scissors enable precise modifications to faulty DNA sequences, potentially curing inherited disorders and even reprogramming cellular responses to malignancies. The advent of bespoke genetic interventions allows clinicians to design therapies based on a patient's unique genomic blueprint, promising enhanced efficacy with minimized toxicity profiles. While the science progresses, ethical frameworks must evolve in parallel to address concerns about germline modifications and long-term ecological impacts.
Pioneering clinical applications demonstrate the viability of genomic corrections for monogenic diseases, suggesting we're entering an era where previously untreatable conditions may become manageable. The technical hurdles of ensuring absolute editing precision and eliminating off-target effects remain significant barriers requiring continued research investment.
Immunotherapy: Revolutionizing Cancer Treatment
The immunotherapy revolution has transformed oncology practice by mobilizing patients' native immune defenses against malignancies. By engineering T-cells or blocking immune checkpoints, these biologics achieve remarkable responses in historically refractory cancers while avoiding traditional chemotherapy's systemic toxicity. The inherent variability of human immune systems creates challenges in predicting individual responses, necessitating sophisticated biomarker development.
Checkpoint inhibitors like PD-1/PD-L1 antagonists represent a watershed moment, delivering durable remissions in metastatic melanoma and lung cancers. While these breakthroughs offer hope, the financial toxicity of treatment and risks of immune-related adverse events demand careful patient selection and monitoring protocols.
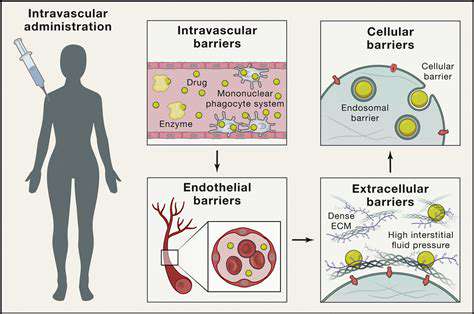
Nanotechnology-Based Drug Delivery Systems
Nanoscale delivery platforms are redefining pharmaceutical pharmacokinetics through precision targeting of diseased tissues. These molecular carriers can encapsulate both small molecules and biologics, dramatically improving therapeutic indices by minimizing off-target exposure. Beyond simple delivery, smart nanoparticles can respond to physiological triggers like pH changes or enzymatic activity for controlled release.
Current investigations explore lipid-based vesicles and polymer conjugates for diverse applications from oncology to neurodegenerative diseases. The translational challenge lies in optimizing biodistribution profiles while ensuring manufacturing consistency at commercial scales.
Personalized Medicine: Tailoring Treatments to the Individual
The precision medicine movement recognizes that effective therapy must account for genomic variability, epigenetic influences, and lifestyle factors. Pharmacogenomic testing now enables clinicians to predict drug metabolism phenotypes, preventing adverse reactions while maximizing therapeutic benefit. This paradigm shift from population-based to N-of-1 treatment strategies represents the future of clinical practice.
While next-generation sequencing costs have decreased dramatically, implementation barriers persist in healthcare systems worldwide, particularly regarding interpretation infrastructure and reimbursement models for genomic medicine services.
Stem Cell Therapies: Regenerating Damaged Tissues
Regenerative medicine approaches utilizing pluripotent cells offer hope for degenerative conditions previously considered irreversible. The ability to differentiate stem cells into functional tissues could address the critical shortage of transplantable organs while avoiding immunosuppression requirements. Current applications in hematologic malignancies and retinal diseases demonstrate proof-of-concept, with numerous other indications under investigation.
Technical challenges remain in ensuring stable engraftment and preventing teratoma formation, while ethical debates continue regarding cell sourcing and genetic manipulation of stem cell lines.
Navigating Ethical Considerations in a Data-Driven World
Data Privacy and Patient Confidentiality
In our era of big data analytics, protecting health information requires multilayered security architectures incorporating blockchain-level encryption and differential privacy techniques. Regulatory frameworks like GDPR and HIPAA establish baseline requirements, but truly ethical data stewardship demands going beyond compliance to implement privacy-by-design principles throughout the research lifecycle.
Transparent consent processes should articulate not just current usage but potential future applications, allowing participants to make truly informed decisions about data sharing. This ethical imperative strengthens public trust in medical research institutions.
Bias in Algorithmic Decision-Making
Machine learning applications in drug development risk perpetuating healthcare disparities if trained on non-representative datasets. Algorithmic audits must become standard practice, evaluating model performance across demographic subgroups to identify potential bias blindspots. Proactive strategies should include oversampling underrepresented populations in training data and developing fairness metrics for model validation.
Intellectual Property and Collaboration
The tension between proprietary interests and open science presents ongoing ethical challenges. Creative licensing frameworks like patent pools and humanitarian clauses can balance commercial viability with global health equity. Precompetitive research consortia demonstrate how structured collaboration can accelerate discovery while protecting legitimate commercial interests.
Transparency and Accountability in Drug Development
Public skepticism toward pharmaceutical innovation often stems from perceived opacity in research practices. Implementing open trial protocols and real-time data sharing platforms can demonstrate commitment to scientific integrity while enabling broader scientific scrutiny. Patient advisory boards should have meaningful input into study design and dissemination plans.
The Role of AI in Ethical Drug Development
While AI promises to revolutionize target identification and clinical trial design, human oversight must remain central to decision-making processes. Explainable AI techniques should elucidate model predictions, and ethical review boards need specialized training to evaluate machine learning applications. Continuous monitoring systems should flag potential algorithmic drift or performance degradation in deployed models.
Data Security and Regulatory Compliance
With cyberthreats growing increasingly sophisticated, zero-trust architectures represent the new security standard for protecting sensitive health data. Beyond technical safeguards, comprehensive staff training programs must create organizational cultures prioritizing data protection. Regular penetration testing and incident response drills ensure preparedness for potential breaches.
Accessibility and Equitable Access to Treatments
The moral imperative of global health justice requires innovative pricing models and technology transfer mechanisms to ensure life-saving innovations reach resource-limited settings. Tiered pricing strategies, voluntary licensing agreements, and public-private partnerships can help bridge the access gap while maintaining sustainable R&D ecosystems.
The Importance of Interdisciplinary Collaboration
The Convergence of Expertise
Modern therapeutic challenges demand synergistic integration of diverse specialties - from molecular biologists to materials scientists and computational modelers. This intellectual cross-pollination sparks unconventional solutions, as demonstrated by recent breakthroughs combining immunotherapy with nanotechnology for enhanced delivery. Physical colocation of researchers from different disciplines in innovation hubs has proven particularly effective at fostering spontaneous collaborations.
Data Integration and Analysis
The exponential growth of multi-omics datasets necessitates new collaborative paradigms between wet-lab scientists and data specialists. Cross-training programs creating bilingual researchers who understand both biological principles and computational methods are proving invaluable. Cloud-based collaborative platforms enable real-time data sharing and analysis across institutional boundaries while maintaining security protocols.
Accelerated Drug Discovery and Development
Convergence science approaches are compressing traditional development timelines through parallel rather than sequential processes. Microphysiological systems developed by engineers, analyzed by computational biologists, and validated by clinicians can simultaneously evaluate efficacy and safety parameters. This integrated approach is particularly valuable for rare diseases where traditional development pathways are economically challenging.
Addressing Complex Diseases
The systems biology perspective essential for understanding multifactorial disorders like diabetes or autoimmune conditions requires sustained collaboration across traditional departmental silos. Network medicine approaches integrating genomic, proteomic, and metabolomic data are revealing previously unrecognized disease subtypes and therapeutic targets. Patient advocacy groups play a crucial role in ensuring research priorities align with lived experience.
Enhanced Innovation and Creativity
Interdisciplinary teams demonstrate increased innovation metrics, as measured by patent filings and high-impact publications. Structured ideation sessions that deliberately combine distant analogies from different fields often yield breakthrough concepts. Institutional support mechanisms like internal seed grants for cross-departmental projects help overcome natural disciplinary inertia.
Ethical Considerations and Responsible Innovation
Embedding ethicists and social scientists in technical teams ensures proactive rather than reactive consideration of societal impacts. This ethics by design approach is particularly crucial for emerging technologies like gene editing and AI-driven diagnostics. Community engagement panels provide valuable reality checks on technological assumptions.
Improving Patient Outcomes
The ultimate measure of successful collaboration is translation to clinical impact. Implementation science teams working alongside basic researchers can identify and overcome real-world adoption barriers early in development. Learning healthcare systems that continuously feed clinical observations back to researchers complete the virtuous cycle of therapeutic innovation.