Hematological malignancies, encompassing a spectrum of cancers affecting the blood and bone marrow, pose significant challenges in terms of diagnosis and treatment. Effective treatment strategies often necessitate a multifaceted approach, leveraging various therapeutic modalities to maximize efficacy and minimize adverse effects. Understanding the complex interplay of genetic and environmental factors contributing to these diseases is crucial for developing innovative interventions.
The development of targeted therapies has revolutionized the landscape of cancer care, offering the potential to precisely inhibit the growth and spread of cancerous cells. This approach contrasts with traditional chemotherapy, which often targets rapidly dividing cells indiscriminately, leading to significant side effects. Consequently, targeted therapies are increasingly employed in the management of hematological malignancies.
Immunotherapy: Harnessing the Body's Natural Defenses
Immunotherapy, a rapidly evolving field, is demonstrating remarkable potential in combating hematological malignancies. This approach involves harnessing the body's immune system to recognize and destroy cancer cells. Strategies include checkpoint inhibitors, adoptive cell therapies, and therapeutic vaccines.
These therapies stimulate the immune response, leading to the elimination of cancerous cells and a potentially improved overall survival rate. This approach is particularly promising for patients with certain types of leukemia and lymphoma.
Targeted Drug Therapies: Precision Medicine in Action
Targeted drug therapies are designed to interfere with specific molecular pathways crucial for the development and progression of hematological malignancies. These therapies often target specific genetic mutations or abnormal signaling pathways that are unique to cancer cells.
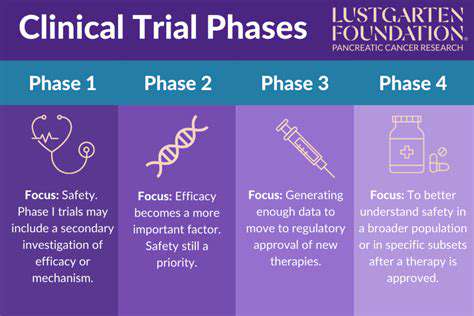
This precision approach minimizes harm to healthy cells, thereby reducing the side effects associated with traditional chemotherapy. Clinical trials are ongoing to further explore the efficacy and safety of these therapies in various hematological malignancies.
Role of Bone Marrow Transplantation: A Powerful Therapeutic Tool
Bone marrow transplantation (BMT) remains a critical therapeutic modality for certain hematological malignancies. It involves replacing diseased bone marrow with healthy donor marrow, providing a chance for hematopoietic recovery. This powerful approach is often employed in cases of acute leukemia or lymphoma.
Careful donor selection and meticulous post-transplantation monitoring are essential to minimize complications and maximize the success of BMT. The long-term outcomes of BMT can vary significantly based on the specific malignancy, donor type, and patient factors.
Combination Therapies: Enhancing Treatment Outcomes
Combination therapies, which involve the use of multiple drugs or therapies in conjunction, frequently yield superior outcomes in treating hematological malignancies. These approaches often target multiple aspects of the disease process simultaneously. The synergistic effects of combining different therapies can lead to increased efficacy and reduced resistance.
Tailoring these combinations to individual patient characteristics is crucial for maximizing the benefits and minimizing the potential side effects. Careful consideration of drug interactions and potential toxicity profiles is vital in the development of personalized treatment strategies.
Supportive Care: Addressing the Holistic Needs of Patients
Supportive care plays a crucial role in the overall management of hematological malignancies. This encompasses a range of services aimed at addressing the physical, emotional, and social needs of patients and their families during and after treatment. This includes symptom management, nutrition counseling, and psychological support.
The provision of comprehensive supportive care is essential to improve the quality of life for patients undergoing treatment for these often debilitating diseases. Addressing the emotional and practical challenges associated with cancer treatment is just as important as the medical interventions.
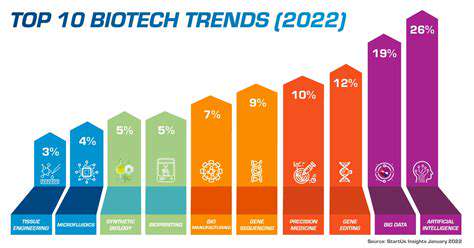
Novel Therapeutic Strategies: Exploring Emerging Approaches
Research into novel therapeutic strategies for hematological malignancies is continuously progressing. Innovative approaches such as gene therapy, immunotherapy, and nanomedicine hold immense promise for improving treatment outcomes and patient survival. These emerging approaches aim to target specific molecular mechanisms driving the disease and enhance the effectiveness of existing therapies.
Ongoing research and clinical trials are paving the way for more effective and personalized treatments for hematological malignancies, offering hope for improved outcomes in the future. These cutting-edge strategies are poised to transform the way we approach these challenging diseases.
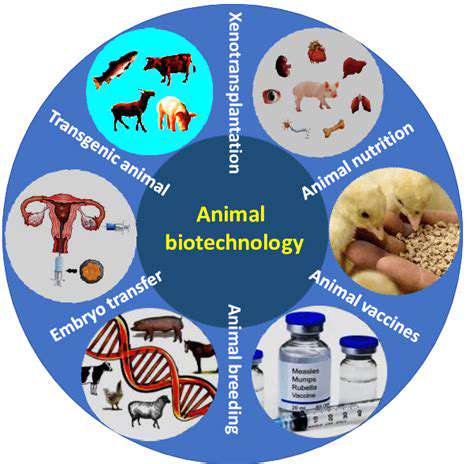
Gene Editing for Inherited Blood Disorders: A Broad Spectrum

Gene Editing Approaches for Inherited Blood Disorders
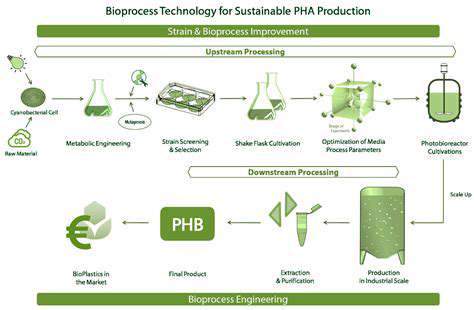
Gene editing technologies, like CRISPR-Cas9, offer revolutionary potential for treating inherited blood disorders. These technologies allow scientists to precisely target and modify specific genes within cells, potentially correcting the genetic defects responsible for these conditions. This precision approach holds the promise of a more permanent and effective cure, compared to traditional treatments. The goal is to correct the underlying genetic flaw, eliminating the need for ongoing therapies.
Different gene editing approaches are being explored, each with its own strengths and limitations. Some methods focus on directly correcting the faulty gene, while others aim to introduce a healthy copy of the gene or to silence a disease-causing gene. The choice of approach depends on the specific genetic mutation causing the disorder.
Targeting Specific Blood Cell Types
Inherited blood disorders often affect specific types of blood cells, such as red blood cells, white blood cells, or platelets. Efficient gene editing requires targeting the relevant blood cell lineages, to ensure that the desired correction takes place in the correct cell type. This is crucial for maximizing therapeutic efficacy and minimizing off-target effects. Researchers are working diligently to develop methods that specifically target and modify these cells.
For example, techniques like inducing pluripotent stem cells (iPSCs) from patients' own cells, and then editing the desired genes in these cells before differentiating them back into the relevant blood cell types, hold significant promise. This approach allows for personalized treatment tailored to each patient's specific genetic makeup.
Delivering Gene Editing Tools
Effectively delivering the gene editing tools to the target cells is a significant hurdle in gene therapy. Different methods are being explored, including viral vectors, which can effectively deliver the gene editing components into cells. Ensuring the delivery system is safe, efficient, and targeted to the specific cells is crucial for the success of gene editing therapies. Further research is needed to optimize these delivery systems for maximum efficacy.
Other non-viral methods are also being investigated, offering potentially safer alternatives to viral vectors. These approaches aim to improve the safety profile and reduce the risk of immune responses.
Ethical Considerations and Future Directions
Gene editing holds immense promise for treating inherited blood disorders, but it also raises important ethical considerations. Issues of accessibility, cost, and potential long-term effects must be carefully addressed to ensure equitable access to these therapies. Thorough preclinical and clinical trials are essential to assess safety and efficacy before widespread use. Further research is needed to fully understand the potential long-term consequences of gene editing.
The future of gene editing for inherited blood disorders is bright, with ongoing research constantly pushing the boundaries of what's possible. Continued advancements in gene editing technologies and delivery methods will likely pave the way for more precise and effective treatments, ultimately improving the lives of those affected by these conditions.
Safety and Off-Target Effects
Safety is a paramount concern in gene editing therapies. Off-target effects, where the editing tool unintentionally modifies other genes, can have serious consequences. Rigorous testing and quality control are essential to minimize these risks and ensure the safety of patients. Scientists are developing strategies to improve the accuracy of gene editing tools and to better understand and mitigate potential off-target effects.
Furthermore, immune responses to the gene editing components or the modified cells can also occur. Strategies to minimize these responses are being explored, including approaches to reduce the immunogenicity of the delivery vectors and gene editing components.
The traditional model of higher education often presents significant barriers for individuals seeking to upskill or advance their careers. Geographical limitations, financial constraints, and inflexible schedules can prevent many from accessing high-quality educational opportunities. AI-powered micro-credential programs offer a flexible and accessible alternative, allowing learners to acquire specific skills and knowledge without the commitment of a full degree program. This democratizing approach is crucial for fostering lifelong learning and promoting social mobility.
Challenges and Future Directions
Off-Target Effects and Immunogenicity
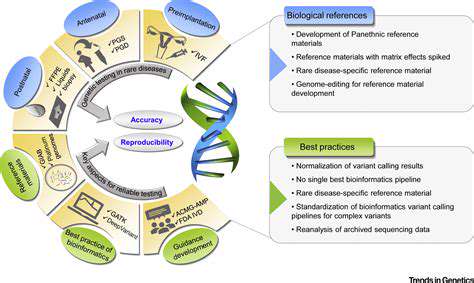
A significant hurdle in gene editing therapies is the potential for off-target effects, where the editing machinery inadvertently alters genes other than the intended target. This can lead to unexpected and potentially harmful consequences, such as the activation of oncogenes or the disruption of crucial cellular pathways. Minimizing these off-target effects is crucial for the safety and efficacy of gene editing therapies, requiring rigorous testing and optimization of the editing tools and delivery methods.
Furthermore, the immune system's response to the introduced genetic material can pose another challenge. The body may perceive the edited cells as foreign, triggering an immune response that could lead to the destruction of the genetically modified cells. Developing strategies to mitigate this immune response, such as modifying the edited cells to reduce their immunogenicity or administering immune-suppressive therapies, is vital for the successful translation of gene editing into clinical practice.
Delivery and Targeting Strategies
Efficient delivery of gene editing tools to the target cells within the hematopoietic system remains a significant challenge. The complex architecture of the bone marrow and the heterogeneous nature of hematopoietic stem and progenitor cells necessitate the development of precise and targeted delivery methods. Nanocarriers, viral vectors, and other delivery systems are being actively explored to enhance the efficiency and specificity of gene editing interventions.
Improving targeting strategies is another crucial aspect. Precise targeting of the desired cell populations is essential to maximize the therapeutic benefit while minimizing off-target effects and adverse reactions. Developing cell-surface markers or other specific targeting mechanisms to guide the gene editing tools to the appropriate cells is a key area of research.
Scalability and Cost-Effectiveness
The current cost of gene editing therapies is often prohibitive for widespread adoption. To facilitate broader access to these potentially life-saving interventions, significant efforts are focused on developing scalable manufacturing processes for gene editing tools and delivery systems. This includes optimizing production methods to reduce costs and increase efficiency.
Furthermore, the long-term cost-effectiveness of gene editing needs careful consideration. While the initial costs may be high, the potential for long-term disease remission and reduced healthcare costs associated with chronic hematological conditions needs to be evaluated. This requires robust long-term follow-up studies to assess the long-term safety and efficacy of these interventions.
Ethical and Societal Considerations
Gene editing technologies raise complex ethical and societal considerations, particularly regarding germline editing. The potential for unintended consequences and the implications for future generations warrant careful ethical review and public dialogue. Establishing clear guidelines and regulations for the development and application of gene editing technologies is essential to ensure responsible innovation and equitable access.
The potential for gene editing to alter the human genome also raises concerns regarding access and equity. Ensuring that these powerful technologies are not used to exacerbate existing health disparities and are available to all in need is crucial.