Fungal infections, encompassing a wide spectrum of diseases, pose a significant and often underestimated threat to human health globally. These infections, ranging from superficial skin conditions to life-threatening systemic diseases, affect people of all ages and socioeconomic backgrounds. Understanding the pervasiveness and varied nature of fungal infections is crucial for developing effective prevention and treatment strategies.
The increasing prevalence of fungal infections is a growing public health concern, particularly in immunocompromised individuals and those with underlying health conditions. This rise is attributed to several factors, including the misuse of antibiotics, the emergence of drug-resistant fungal strains, and the growing prevalence of environmental factors that promote fungal growth.
The Diverse Spectrum of Fungal Pathogens
The fungal kingdom is incredibly diverse, harboring numerous species that can cause a wide array of infections. Some fungi are opportunistic pathogens, meaning they typically do not cause disease in healthy individuals but can lead to severe infections in those with weakened immune systems. Other fungi are considered primary pathogens, meaning they can cause disease in otherwise healthy individuals.
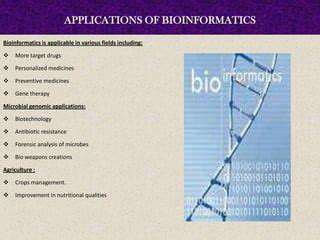
This vast array of fungal species and their diverse infection mechanisms underscores the complexity of fungal diseases and the need for specialized diagnostic tools and treatment approaches.
Risk Factors and Predisposing Conditions
Several factors can increase a person's susceptibility to fungal infections. These include weakened immune systems, such as those found in individuals with HIV/AIDS, cancer, or organ transplant recipients. Certain medications, particularly broad-spectrum antibiotics, can disrupt the delicate balance of the body's microbiota, creating an environment conducive to fungal overgrowth.
Diabetes, and other chronic illnesses, can also increase the risk of fungal infections. Exposure to contaminated environments, particularly in healthcare settings or during travel, can also play a role.
Diagnosis and Treatment Strategies
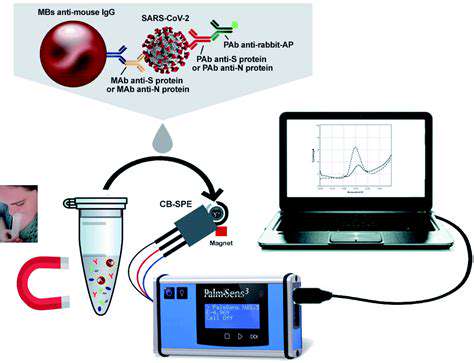
Accurate diagnosis of fungal infections is often challenging, requiring specialized laboratory tests to identify the specific fungal species involved. Microscopic examination of infected tissues, cultures, and molecular techniques are crucial for accurate diagnosis. Early detection is essential to initiate appropriate treatment and prevent the spread of infection.
Treatment options vary significantly depending on the type of fungal infection and the individual's overall health. Antifungal medications, available in various forms, represent the cornerstone of treatment, but resistance to these drugs is a growing concern.
Prevention and Public Health Measures
Preventive measures are essential to minimize the risk of fungal infections. Maintaining good hygiene practices, particularly in healthcare settings, is crucial to prevent the spread of fungal pathogens. Promoting healthy immune systems through a balanced diet, regular exercise, and stress reduction is also important for overall immune function and resilience to fungal infections.
Public health campaigns focused on raising awareness about fungal infections and risk factors can empower individuals to take preventive actions and promote early detection.
Emerging Trends and Future Directions
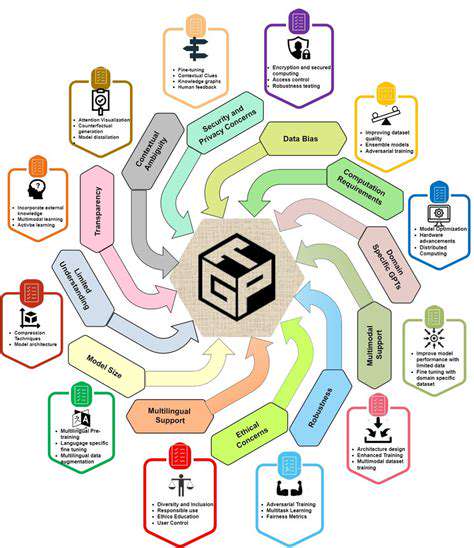
The landscape of fungal infections is constantly evolving, with emerging fungal pathogens and drug resistance posing significant challenges. Research efforts are crucial to understand the mechanisms of fungal pathogenesis and develop new diagnostic tools and therapeutic strategies. Continued monitoring and surveillance of fungal infections are needed to identify emerging trends and adapt public health measures accordingly.
Further research into antifungal drug development, novel diagnostic technologies, and preventive strategies is vital for addressing the pervasive threat of fungal infections in the future.

The traditional classroom model is rapidly evolving, with online learning platforms becoming increasingly sophisticated and accessible. This shift offers unparalleled flexibility for students, enabling them to learn at their own pace and from anywhere with an internet connection. Online courses are no longer just a supplementary option; they are becoming a primary method of education for many, offering a wider range of courses and specialized programs. This accessibility also extends to students in remote areas or those with disabilities, creating a more inclusive learning environment.
Targeting Unique Fungal Pathways: A Precision Approach

Targeting Fungal Cell Wall Synthesis
Fungal cell walls, unlike those of animal cells, are composed primarily of chitin, a complex polysaccharide. Targeting enzymes involved in chitin synthesis presents a promising avenue for antifungal drug development. Disrupting this crucial process can effectively inhibit fungal growth without significantly impacting human cells, as human cells lack chitin. This approach leverages the fundamental differences between fungal and human cell structures to minimize adverse side effects.
Furthermore, focusing on specific enzymes in the chitin synthesis pathway allows for the development of highly targeted therapies. This specificity enhances the likelihood of effective treatment while reducing the risk of resistance development. Specific inhibitors could be designed to target key steps in the process, thereby hindering fungal growth.
Inhibiting Fungal Metabolism
Fungi require specific metabolic pathways to thrive. Targeting these pathways, particularly those involved in essential nutrient uptake or energy production, can interrupt fungal viability without harming human cells. Identifying and inhibiting key enzymes in these metabolic processes can lead to effective antifungal agents.
For instance, inhibiting the enzymes responsible for utilizing specific nutrients critical for fungal growth could effectively starve the fungi, preventing their proliferation. This approach offers a novel strategy for antifungal therapies, focusing on the unique metabolic requirements of the fungi.
Interfering with Fungal Protein Synthesis
Fungal protein synthesis shares some similarities with human protein synthesis, but crucial differences exist. Targeting these disparities in the process could be a powerful approach. By specifically inhibiting enzymes or ribosomes involved in fungal protein synthesis, antifungal agents could effectively disrupt the fungal cell's ability to produce essential proteins. This disruption can effectively halt fungal growth without harming human cells.
Developing inhibitors targeting the fungal ribosomes or specific steps in the protein synthesis pathway could offer a new class of antifungal agents. This targeted approach might prove effective in combating fungal infections while minimizing the risk of toxicity in humans.
Disrupting Fungal DNA Replication and Repair
Fungal DNA replication and repair mechanisms differ significantly from those in humans. Exploiting these differences to develop antifungal agents could prove highly beneficial. Targeting specific enzymes or pathways involved in DNA replication or repair in fungi could disrupt their growth and survival. This approach aims to selectively inhibit fungal DNA synthesis, a process essential for fungal replication.
Identifying unique fungal DNA replication or repair enzymes could lead to the development of new antifungal drugs. Furthermore, these targeted approaches could help circumvent the development of resistance compared to broad-spectrum antifungal agents. This strategy could offer a powerful tool in combating fungal infections.