Gene Editing for Hearing Loss: CRISPR-Cas9
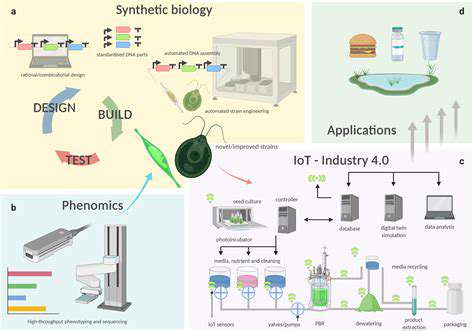
CRISPR-Cas9 technology, modeled after bacterial defense mechanisms, represents a breakthrough in potential hearing loss treatments. This system enables precise modification of specific DNA sequences, offering hope for correcting mutations that cause inherited hearing disorders. By targeting affected cells, researchers aim to repair faulty hearing genes, potentially surpassing traditional treatment limitations.
Beyond therapeutic applications, CRISPR-Cas9 provides valuable research tools. Scientists can systematically alter genes to study their roles in hearing, deepening understanding of auditory system function. These insights may lead to more refined and effective treatment strategies.
Beyond CRISPR: Other Gene Editing Tools
While CRISPR-Cas9 dominates current discussions, alternative gene editing methods are emerging. Base editors enable single-base DNA modifications without disrupting the double helix, while prime editors permit more complex genetic changes. These alternatives may offer improved precision and reduced unintended effects, making them attractive options for future therapies.
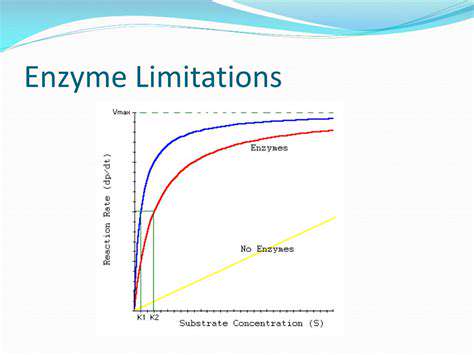
These novel techniques could overcome CRISPR's limitations, particularly regarding accuracy and delivery challenges. Developing more precise editing tools remains critical for creating safer, more effective hearing loss treatments.
Ethical Considerations and Future Directions
Gene editing applications for hearing loss raise significant ethical questions that require careful consideration. Balancing potential benefits against possible risks demands thorough evaluation and responsible implementation. Public discourse and robust regulatory frameworks must guide therapeutic development to ensure safety, accessibility, and equitable distribution.
The future of hearing loss treatment appears promising as research advances. Improved understanding of hearing loss causes combined with evolving gene editing technologies may yield more effective, minimally invasive treatments. Realizing this potential depends on continued innovation in delivering editing tools to inner ear cells safely and efficiently.
Potential Challenges and Future Directions
Off-Target Effects and Safety Concerns
A primary challenge in hearing loss gene therapy involves unintended genetic modifications. Even precise editing tools may occasionally alter non-target genes, potentially causing adverse effects. Extensive preclinical testing and careful patient monitoring remain essential before clinical adoption.
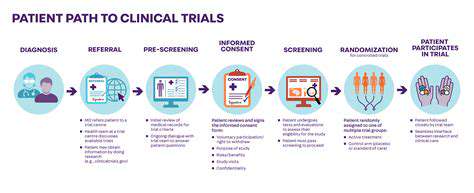
Safety remains the foremost priority in developing gene therapies. Researchers must refine editing precision and study long-term effects on auditory development through comprehensive animal studies and clinical trials.
Delivery Methods and Accessibility
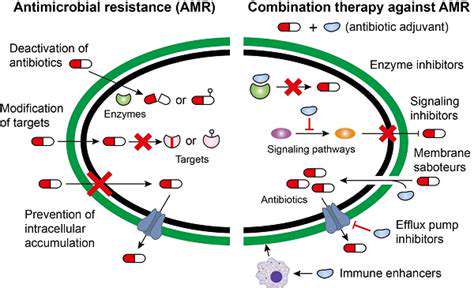
The inner ear's complex anatomy presents significant delivery challenges for gene therapies. Scientists are evaluating various approaches, including viral carriers and nanoparticle systems, to effectively transport editing tools to target cells. Ensuring these methods' safety and efficacy requires thorough investigation.
Equitable access to these advanced treatments represents another critical consideration. Developing cost-effective production methods and innovative funding models will be essential for making therapies widely available.
Ethical Considerations and Public Perception
Gene editing applications for inherited conditions like hearing loss involve complex ethical dimensions. Society must address questions about consent, social implications, and fair treatment access to ensure responsible implementation and prevent exacerbating inequalities.
Long-Term Effects and Monitoring
The extended consequences of hearing loss gene therapies remain largely unknown. Longitudinal studies must track treatment efficacy, potential side effects, and overall patient health over many years to fully understand these interventions' impacts.
Integration with Existing Therapies
Combining gene editing with conventional treatments like hearing aids or implants could offer comprehensive hearing loss management. Exploring synergistic approaches may yield more effective solutions than any single treatment method.
Research Funding and Collaboration
Sustained research investment and international cooperation will accelerate progress in hearing loss gene therapy. Sharing knowledge and resources among scientists, clinicians, and industry partners can drive innovation and translate discoveries into clinical applications more rapidly.
Ethical Considerations and Public Health Implications

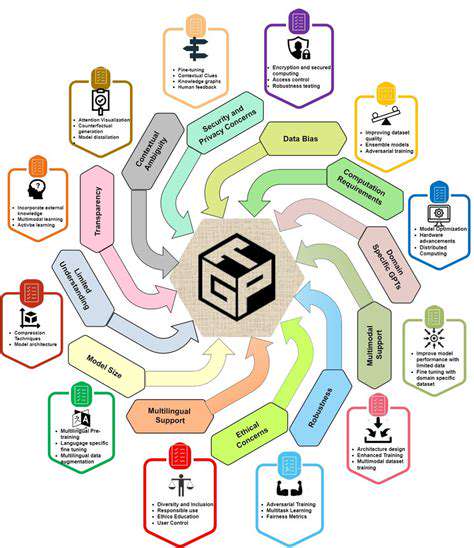
Transparency and Accountability
Open communication about research methods and data handling forms the foundation of ethical scientific practice. Participants deserve clear explanations about study purposes, data usage, and access protocols. Maintaining rigorous documentation of research processes ensures accountability and fosters public confidence.
Researchers must also disclose any potential conflicts of interest that might influence their work, including financial relationships or personal biases that could affect study outcomes.
Protecting Vulnerable Populations
Special ethical considerations apply when researching hearing loss in vulnerable groups like children or individuals with disabilities. Researchers must implement additional safeguards to protect these participants, ensuring their well-being remains the top priority throughout the study. This includes developing consent processes tailored to participants' specific needs and comprehension levels.
Community engagement and cultural sensitivity become particularly important when working with marginalized populations to ensure respectful and appropriate research practices.
Data Privacy and Security
Protecting participant data requires implementing robust security measures, including encrypted storage systems and strict access controls. Anonymizing data whenever possible helps minimize privacy risks while maintaining research utility.
Data security represents both a legal obligation and moral responsibility for researchers. Preventing unauthorized access protects participants from potential harm while maintaining research integrity.
Informed Consent and Participant Rights
True informed consent requires providing comprehensive study information in understandable terms, including potential risks and benefits. Participants must retain the right to withdraw at any time without consequence.
Respecting participant autonomy means ensuring they have all necessary information to make voluntary, educated decisions about their involvement. Researchers should encourage questions and confirm comprehension before proceeding.
Conflicts of Interest and Bias
Researchers must proactively identify and disclose any factors that could compromise their objectivity, including funding sources or personal convictions that might influence their work.
Minimizing bias requires rigorous methodology, diverse perspectives, and constant self-evaluation throughout the research process. Awareness of potential biases helps researchers maintain scientific integrity.
Dissemination and Impact
Responsible research communication involves sharing findings with all relevant stakeholders in accessible formats. Researchers should consider how their work might be interpreted and applied in various contexts.
Ethical research dissemination can drive positive societal change when conducted thoughtfully. Researchers must anticipate potential consequences and address concerns that may arise from their published work.