Diverse Manifestations and Symptoms
The clinical presentation of autoimmune disorders varies as widely as human physiology itself, creating diagnostic puzzles for healthcare providers. These conditions can target any bodily system, producing an astonishing range of clinical pictures. Patients may experience anything from persistent exhaustion and articular discomfort to dermatological eruptions and vital organ impairment, with symptom intensity and chronicity differing dramatically between individuals.
The spectrum of autoimmune pathology demonstrates remarkable variety. While some disorders primarily drive systemic inflammatory processes, others generate specialized antibodies that assault particular anatomical structures. This heterogeneity underscores the necessity for clinicians with specialized training in autoimmune pathology recognition and management protocols.
Genetic Predisposition and Environmental Factors
Inherited biological markers substantially influence autoimmune disease vulnerability. Specific genetic sequences elevate disease probability, though external elements frequently serve as critical co-factors. Pathogen encounters, chemical exposures, and nutritional components all participate in triggering and modulating autoimmune pathways. The dynamic relationship between hereditary factors and environmental stimuli forms the foundation for both preventive measures and therapeutic innovations.
Diagnostic Challenges and Advancements
Identifying autoimmune conditions presents unique difficulties due to symptom overlap with numerous other medical issues. Comprehensive diagnosis typically requires multifaceted assessment incorporating clinical examination, specialized laboratory analysis, and advanced imaging modalities. Modern diagnostic technology has revolutionized detection capabilities, enabling faster, more precise identification that facilitates timely treatment initiation and enhanced recovery trajectories.
Treatment Approaches and Therapies
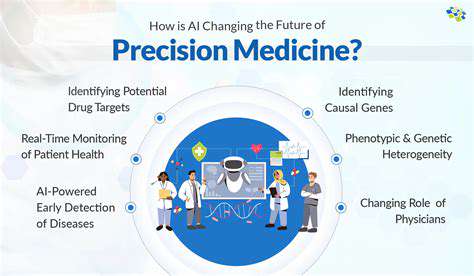
Contemporary autoimmune disease management focuses on three primary objectives: symptom control, immune response modulation, and tissue protection. Treatment regimens commonly integrate pharmaceutical compounds, behavioral adjustments, and complementary support modalities. Medications including corticosteroid preparations and immune-suppressing agents remain fundamental for inflammation management and disease course alteration. Investigational therapies exploring precision immunomodulation and cellular interventions promise more targeted treatment paradigms with potentially superior efficacy profiles.
The Impact on Quality of Life
Chronic autoimmune conditions profoundly affect patients' daily existence and functional capacity. The persistent nature of these disorders frequently leads to energy depletion, discomfort, and movement limitations. Psychological burdens associated with long-term illness management can substantially influence emotional stability and interpersonal relationships. Dedicated support networks and educational resources prove invaluable for enhancing coping strategies and overall wellness in affected individuals and their families.
Targeting Specific Genes in Autoimmune Diseases
Gene Editing Strategies for Autoimmune Diseases
CRISPR-Cas9 and related genomic modification technologies represent a paradigm shift in autoimmune disease intervention. These scientific tools enable unprecedented precision in altering disease-associated genetic sequences. The capacity to rectify malfunctioning genes responsible for immunological imbalance marks substantial progress toward addressing disease origins rather than merely managing symptoms.
Through selective genetic modification of immune regulation pathways, researchers anticipate restoring proper immunological function while preventing inappropriate tissue targeting. This precision-oriented methodology may reduce complications associated with conventional broad-spectrum immunosuppression. Such technological developments are catalyzing personalized medical approaches customized to individual genetic architectures.
Identifying Key Genes in Autoimmune Processes
Successful genetic intervention requires accurate identification of pivotal autoimmune-related genes. Investigators are systematically mapping the intricate genetic networks governing immune regulation, inflammatory cascades, and tissue injury mechanisms. This intensive research incorporates comprehensive genetic association studies, nucleotide sequence analysis, and functional genomic investigations to isolate critical disease-driving genetic elements.
Detailed understanding of condition-specific genetic pathways is fundamental for developing effective editing protocols. This knowledge base permits targeted modification of primary disease-causing genes, optimizing therapeutic potential while minimizing collateral genetic effects. Precise genetic target identification forms the essential foundation for designing customized autoimmune disease interventions.
Delivery Systems for Gene Editing Tools
Effective therapeutic application requires reliable transport mechanisms for genetic modification components to affected cell populations. Current research explores multiple delivery platforms including engineered viral carriers, synthetic transport vehicles, and nanoscale particulate systems, each offering distinct advantages regarding cellular targeting precision and biological safety.
Developing robust delivery methodologies constitutes a major translational challenge for clinical implementation. Continuous refinement of these systems aims to enhance target cell specificity while reducing unintended genetic alterations and potential toxic effects. Overcoming these delivery obstacles remains critical for realizing the full clinical potential of genetic editing technologies.
Potential Benefits and Challenges of Gene Editing
Genetic modification technology offers transformative possibilities for autoimmune disease management through precise immunological recalibration. By addressing fundamental genetic abnormalities, these approaches may provide durable disease modification surpassing conventional treatment limitations. Comprehensive longitudinal studies remain essential to fully characterize treatment durability and potential late-emerging effects.
Ethical considerations regarding genetic manipulation, particularly heritable modifications, demand careful societal deliberation. Establishing responsible usage guidelines and equitable access frameworks will be crucial as these technologies advance toward clinical reality. While therapeutic potential appears considerable, balanced evaluation of both scientific and ethical dimensions will ensure appropriate integration into medical practice.