Harnessing the Power of Genomics and Omics Technologies
Genomics in Antibiotic Discovery
Genomics, the study of an organism's complete set of DNA, plays a crucial role in understanding bacterial pathogens and developing effective antibiotics. Analyzing bacterial genomes reveals unique genetic markers and pathways that can be targeted for drug development. Identifying specific genes or metabolic processes essential for bacterial survival but absent or different in human cells is vital for designing antibiotics that selectively inhibit bacterial growth without harming the host. This approach allows scientists to tailor antibiotic therapies to specific bacterial strains, minimizing the risk of resistance development.
Comparative genomics, which contrasts bacterial genomes with those of humans, can also reveal critical insights. By pinpointing differences in genetic sequences and functions, researchers can identify potential drug targets with minimal impact on human cells. This knowledge facilitates the development of more effective and safer antibiotics.
Omics Technologies for Target Identification
Omics technologies, encompassing genomics, transcriptomics, proteomics, and metabolomics, offer a comprehensive view of biological systems. These technologies provide a powerful arsenal for discovering novel drug targets, revealing intricate molecular pathways involved in bacterial infection and survival. Transcriptomics, for example, analyzes gene expression patterns in response to environmental changes, including antibiotic exposure, offering insights into the bacteria's response mechanisms. This knowledge can be crucial for designing antibiotics that target these response pathways, potentially preventing resistance development.
Drug Target Validation and Characterization
Once potential drug targets are identified, meticulous validation and characterization are crucial. This involves experimentally confirming the target's role in bacterial function and ensuring its suitability for drug intervention. Validation studies often involve inhibiting the target using specific inhibitors and observing the effect on bacterial growth and viability. This rigorous process ensures that the selected targets are truly essential for bacterial survival and have minimal impact on human cells, minimizing potential toxicity issues.
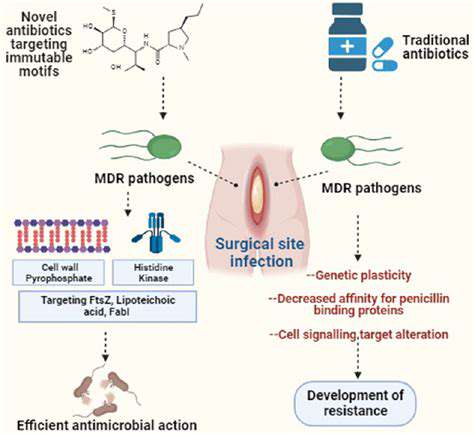
Antibiotic Resistance Mechanisms
Understanding the mechanisms by which bacteria develop resistance to antibiotics is paramount in the fight against antimicrobial resistance. Genomics and other omics technologies can pinpoint the genetic mutations and alterations that confer resistance. By analyzing the genetic changes associated with resistance, scientists can design antibiotics that circumvent these mechanisms or target alternative pathways essential for bacterial survival. This knowledge is crucial for developing new generations of antibiotics that are resistant to existing resistance mechanisms.
Developing Novel Antibiotic Classes
Genomics and omics technologies facilitate the discovery of novel antibiotic classes by identifying previously unexplored targets in bacterial pathogens. These targets may involve enzymes, proteins, or metabolic pathways critical for bacterial survival and growth, but absent or different in human cells. This approach can lead to the development of entirely new classes of antibiotics with unique mechanisms of action, potentially overcoming the limitations of existing drugs and combating the growing threat of antibiotic resistance. This innovative approach is essential for expanding the antibiotic armamentarium and ensuring effective treatment options for bacterial infections.
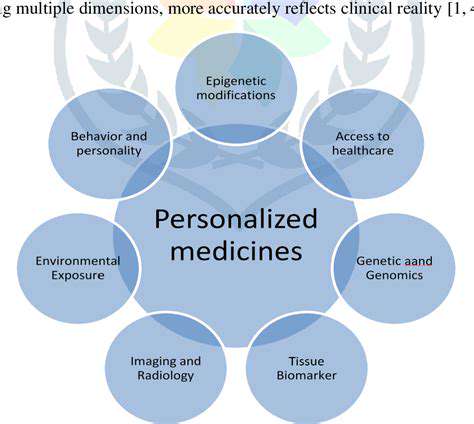
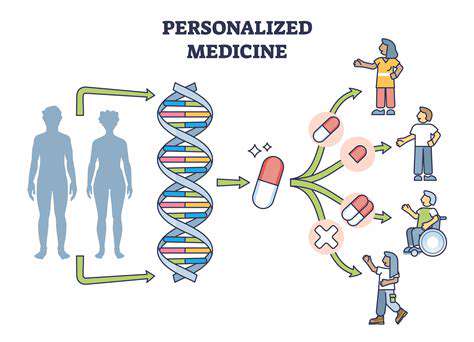
Personalized Antibiotic Therapy
In the future, personalized antibiotic therapy may become a reality, tailored to the specific genetic makeup of each individual patient and the infecting bacterial strain. Genomic analysis of both the patient and the pathogen can provide invaluable information for selecting the most effective and least toxic antibiotic. This approach could reduce the risk of adverse effects and promote faster recovery times. Furthermore, it could potentially limit the development of antibiotic resistance by using targeted therapies for each specific infection.
Developing New Drug Delivery Systems for Enhanced Efficacy
Improving Drug Absorption
A crucial aspect of developing effective drug delivery systems is enhancing the absorption of the drug into the bloodstream. This can be achieved through various strategies, including the use of novel drug formulations that improve solubility and permeability across biological membranes. For instance, nanoparticles can encapsulate drugs, increasing their surface area for interaction with the target site and thereby facilitating absorption. This targeted approach minimizes the need for high drug dosages, reducing potential side effects and improving the overall therapeutic outcome.
Another key consideration is the specific route of administration. Different routes, such as oral, intravenous, or transdermal, have varying absorption characteristics. Developing drug delivery systems tailored to these specific routes can significantly enhance drug bioavailability. This involves optimizing the physical and chemical properties of the drug and carrier to ensure efficient transport to the target site.
Targeted Drug Delivery
Targeted drug delivery systems aim to deliver the therapeutic agent directly to the diseased cells or tissues, minimizing damage to healthy cells. This precision approach is particularly important for cancer therapies, where the goal is to destroy cancerous cells while preserving healthy tissues. Utilizing specific targeting molecules, such as antibodies or peptides, conjugated to the drug carrier can direct the drug to the desired location, enhancing therapeutic efficacy and reducing side effects.
Nanotechnology plays a significant role in achieving targeted drug delivery. Nanocarriers, such as liposomes and polymeric nanoparticles, can be engineered to carry drugs and deliver them to specific cells or tissues. This approach can improve drug efficacy by increasing the concentration of the drug at the target site and reducing the systemic exposure, thus decreasing the adverse effects.
Sustained Drug Release
Sustained drug release systems are designed to release the drug over an extended period, maintaining therapeutic concentrations in the body. This approach can improve patient compliance by reducing the frequency of administrations. Developing sustained-release formulations often involves utilizing controlled release mechanisms, such as polymeric matrices or liposomal systems, that gradually release the drug over time. This consistent release profile ensures a more stable therapeutic effect and minimizes fluctuations in drug levels in the body.
Enhancing Drug Stability
Drug stability is a critical factor in drug development, and drug delivery systems need to protect the drug from degradation during storage and administration. This is especially important for drugs that are susceptible to environmental factors like light, heat, or moisture. Developing robust formulations that protect drugs from degradation is essential to maintain their efficacy and ensure the quality of the final product. This can involve using specialized coatings, incorporating stabilizing agents, or optimizing the manufacturing process.
Improving Drug Solubility
Many drugs have poor water solubility, which limits their absorption and bioavailability. Developing drug delivery systems that improve drug solubility is crucial for enhancing their efficacy. This can involve using solubilizing agents, such as surfactants or cosolvents, or designing drug formulations that increase the surface area of the drug for interaction with the aqueous environment. These approaches can significantly improve the absorption of poorly soluble drugs and lead to better therapeutic outcomes.
Minimizing Side Effects
A key consideration in drug delivery system design is minimizing the potential side effects of the drug. By tailoring the drug delivery system to target specific cells or tissues, we can reduce the exposure of healthy cells to the drug and thus minimize unwanted effects. This approach is particularly important in treating diseases where off-target effects can cause significant harm. Drug delivery systems also play a role in reducing the toxicity of drugs, improving their safety profile, and enhancing the overall patient experience.
Overcoming Biofilm Resistance
Biofilms, complex communities of microorganisms, can pose a significant challenge for drug delivery, often hindering the penetration of drugs to infected sites. Developing drug delivery systems that can effectively penetrate and disrupt biofilms is critical for combating infections. This might involve using nanoparticles that can target specific components of the biofilm or utilizing drug delivery systems that can release drugs at a sustained rate to combat the biofilm's resistance mechanisms. Overcoming biofilm resistance is a vital area of research for developing more effective and safer antimicrobial therapies.